Virus transmission
Virus infection in a host is the result of virus replication within individual cells, as described in the previous section. To initiate an infection, viruses must gain access to susceptible cells within a host and in order to persist and evolve viruses need to be able to infect a large population of susceptible hosts. Entry into and transmission (spread) between hosts can occur by a number of routes, most of which are classed as horizontal transmission routes, i.e. transmission between individuals of a family, group or population.
Many viruses gain entry via the respiratory route, including influenza viruses and the rhinoviruses (many of which cause the common cold), coronaviruses (e.g. SARS), and respiratory syncytial virus (RSV). Following inhalation within droplets or dust, viruses can infect and replicate in the epithelial cells of the upper or lower respiratory tract mucosal membranes. The host responds (after several days) with the characteristic symptoms of sneezing and coughing, which of course transmit virus to new hosts. An important respiratory pathogen of infants, RSV infection remains localized at the site of entry, causing severe necrosis of the bronchiolar epithelium. The infected cells slough off, blocking the small airways and leading to obstruction of air flow and respiratory disease. A number of viruses that enter and exit the host via this route are not respiratory viruses and spread beyond the respiratory tract to set up infection (and symptoms) in the cells of the blood or other target organs. These may be viewed as systemic infec- tions and examples include the measles, rubella (German measles) and varicella-zoster
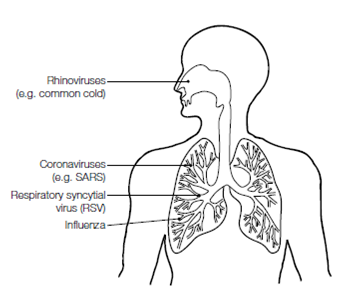
Figure : Routes of infection in the respiratory tract. Virus infections can produce a variety of respiratory disorders, depending on the area of respiratory tract infected.
(Chickenpox) viruses. The measles virus replicates in local lymph nodes that drain from the infected respiratory tissue. The virus enters the blood (primary viremia) where it replicates in the cells of epithelial surfaces before entering the blood again (secondary viremia). At this point the patient is highly infectious but does not have the distinctive measles rash, which appears about 14 days post infection.
The oral–gastrointestinal mucosa is a port of entry used mainly by those viruses responsible for gut infections, such as rotavirus, Norwalk virus, and the Enteroviruses, which include poliovirus. Vast numbers of virus particles can be excreted in fecal material (e.g. in the order of 1012 particles per gram), facilitating the easy spread of these viruses in conditions of poor sanitation. The drinking of fecally contaminated water and consumption of contaminated shellfish or other food prepared by unhygienic food handlers are ways in which these viruses are spread. The skin normally provides an impenetrable barrier to pathogen invasion, but a range of viruses can enter following trauma to the skin. Often this is a wound such as that from an animal bite (rabies virus) or insect bite (yellow fever and dengue viruses). Several viruses are carried by an insect vector such as the mosquito or tsetse fly, and are commonly referred to as arboviruses (arthropod-borne viruses). Other viruses penetrate the skin via contaminated needles during injections, needle- stick injuries or intravenous drug abuse, and these include HIV and the hepatitis B and hepatitis C viruses. These viruses can also be transmitted by iatrogenic routes; infection as a result of medical interventions such as the transfusion of contaminated blood or blood products or the use of unsterilized surgical equipment. In addition to these routes, sexual transmission of viruses is an important mechanism of spread, and viruses such as HSV, HPV, hepatitis B, and HIV can infect hosts in this manner too.
Viruses may also be transmitted vertically – that is, from mother to offspring via the placenta, during childbirth, or in breast milk. Rubella virus (German measles) and cytomegalovirus (CMV) acquired by the mother during pregnancy are easily transmitted to the developing embryo and often lead to severe congenital abnormalities and/or spon- taneous abortion. Some viruses, such as HSV, can infect the developing fetus in utero or during birth and subsequently present as an acute disease syndrome in the neonate.
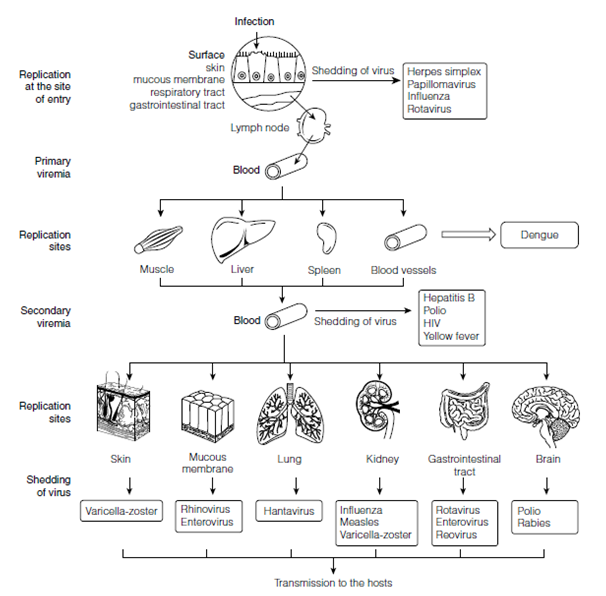
Figure 2. Virus spread within the host. Different viruses have different modes of spreadwithin the host. Some viruses remain localized at the site of entry, whereas others may spread to involve other tissues. Routes of infection are shown, together with examples of possible clinical outcomes. Possible sites of replication are shown and some are also sites of shedding and transmission.
In the case of HIV and hepatitis B, virus transmission in this way means that the neonate may be born with an asymptomatic infection with the virus persisting in a carrier state and developing into disease much later. HIV has also been shown to infect the offspring of infected mothers by way of breast milk.
the case of HIV and hepatitis B, virus transmission in this way means that the neonate may be born with an asymptomatic infection with the virus persisting in a carrier state and developing into disease much later. HIV has also been shown to infect the offspring of infected mothers by way of breast milk.