Pain pathways
The projection neurons in laminae I and II are nociceptor specific. Conduction in Aδ mechanical nociceptor afferents is faster than in C fiber polymodal nociceptor afferents so a painful blow produces a sharp fast pain initially, followed by an aching slow pain.Fast and slow pain is processed separately. There are three pain pathways:
- The spinothalamic tract (STT) mediates fast, well-localized, well-characterized pain. It arises from neurons in laminae I, II, IV, and V, axons of which cross over and ascend on the contralateral side to the posterior (I and II) and ventroposterolateral (IV and V) nuclei of the thalamus. Thalamic neurons project to the primary somatosensory cortex (SI). The somatosensory cortex is assumed to mediate pain localization and discrimination, though it has no pain map.
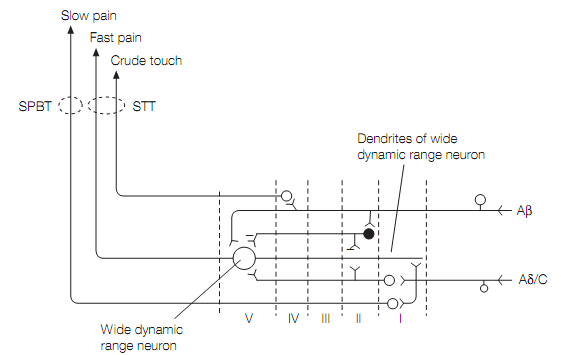
The largest number of spinothalamic tract cells is in lamina V. Their dendrites extend into lamina I and receive inputs from Aδ (fast pain) afferents. But lamina V neurons also receive connections from large diameter (Aβ) mechanoreceptor afferents so are said to be wide dynamic range (WDR) cells, because they get inputs from low threshold and high threshold afferents as shown in figure. Hence most spinothalamic tract neurons can be excited by both innocuous and noxious stimuli. In contrast, lamina IV cells get input only from large diameter (Aβ) mechanoreceptor afferents, and not from nociceptor afferents.
- The spinoreticular tract (SRT) arises from lamina V–VII and makes bilateral connections with reticular nuclei in the brainstem, home to second order neurons that project to reticular (intralaminar) nuclei of the thalamus. These nuclei project to SI, and also to the insula, anterior cingulate cortex and prefrontal cortex—regions involved in emotional and cognitive responses to pain. Interestingly, brain imaging shows that parts of the insula and anterior cingulate are activated by watching pain inflicted on a loved one. Activation of brainstem reticular nuclei generates autonomic responses to pain (e.g., increases in heart rate and blood pressure) and changes in ventilation. In particular, by activating noradrenergic neurons in the locus coeruleus the SRT increases arousal. Finally, the thalamic nuclei make connections with the basal ganglia, influencing motor activity.
- The spinoparabrachial tract (SPBT) arises from lamina I cells that get their input from C fiber (slow pain) afferents and synapse with cells in the parabrachial nucleus that project to the hypothalamus and amygdala. Via these connections pain activates pituitary–adrenal axis stress responses, affects appetitive (eating and drinking) behavior and sleep, and mediates fear learning.All three pain pathways receive input from visceral afferents as well as skin nociceptors, but visceral nociceptors also terminate on dorsal horn cells that project to dorsal column nuclei. Pain pathways mediate visceral reflexes but visceral pain perception is exclusively due to the dorsal column–medial lemniscal system.
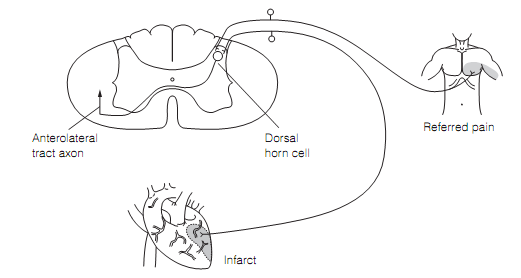
Convergence of visceral and somatic nociceptor afferents onto the same neuron means that stimulation of nociceptors in internal organs is perceived as pain in muscle and skin some distance away. This is referred pain and the areas to which it is referred (Head’s zones) are reliable enough to be useful in diagnosis as shown in figure.
Neurons equivalent to laminae I and V cells in the spinal cord are also found in the spinal nucleus of the trigeminal nerve, that get their inputs from the primary afferents of the face and head. These projects to the ventroposteromedial and posterior thalamic nuclei and are the face and head equivalent of the STT.