ANS physiology
The allocation of the ANS to target organs is as shown in figure below. Acetylcholine (ACh) is the main neurotransmitter at all autonomic ganglia. The ACh discharged from preganglionic neurons acts on nicotinic cholinergic receptors to generate a fast excitatory postsynaptic potential (epsp) that, if adequately large, makes the postganglionic cell fire. Additionally ACh acts on M1 muscarinic receptors genertaing a slow epsp—extending the firing of the postganglionic cell by numerous seconds—by closing a population of potassium (KM) channels. In this manner long-lasting autonomic responses are produced by short stimuli.
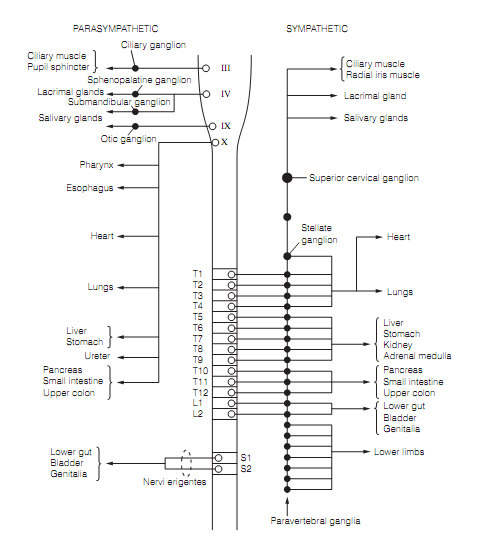
Figure: Distribution of the ANS to target organs.
Nearly all terminals of the sympathetic postganglionic axons secrete noradrenaline (nor-epinephrine), the only significant exception in humans being the cholinergic sympathetic provide to sweat glands. Adrenal medulla chromaffin cells are observed as a postganglionic component of the SNS and secrete adrenaline directly into the blood as an outcome of activity in the preganglionic sympathetic fibers that supply it. There are four main kinds of adreno-receptors which mediate the diverse effects of sympathetic stimulation. They are all GPCRs and their properties are reviewed in table shown below.
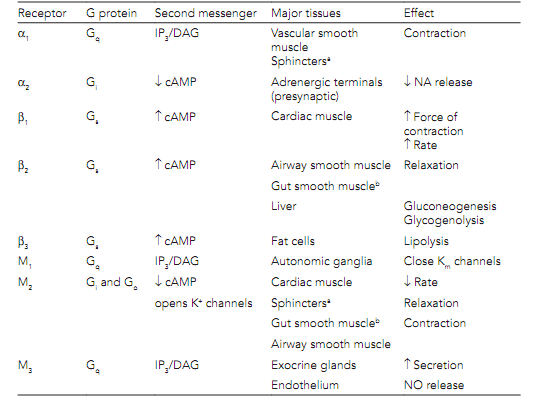
Table: Properties of muscarinic receptors and adrenoceptors and their principal actions at ANS targets
All parasympathetic postganglionic axons discharge ACh, the effects of which are brought around by muscarinic cholinergic (mAChR) receptors. There are numerous subtypes of mAChR, all GPCRs that account for the various effects of parasympathetic activity as shown in table.
Autonomic nerve terminals, in addition to secreting noradrenaline or ACh, also discharge ATP and peptides as co-transmitters. ATP, for illustration, acts on the smooth muscle of blood vessels to generate rapid excitatory postsynaptic potentials and fast contraction. This is followed by a slower response due to noradrenaline. Peptide co-transmitters involve neuropeptide Y (NPY) and vasoactive intestinal peptide (VIP). They extend and modulate the effects of the main transmitter. For illustration, NPY in sympathetic terminals improves the vasoconstrictor response to noradrenaline. VIP from parasympathetic terminals on salivary glands causes vasodilation that enables ACh to generate a greater salivary secretion.