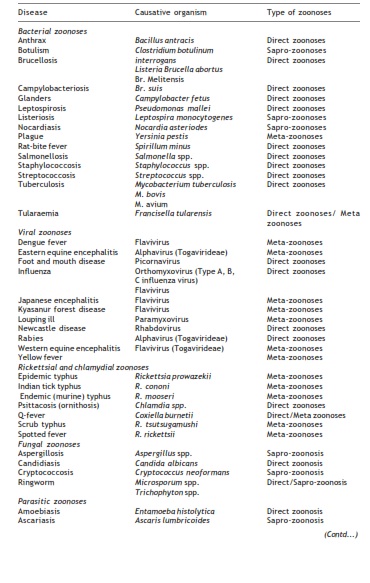
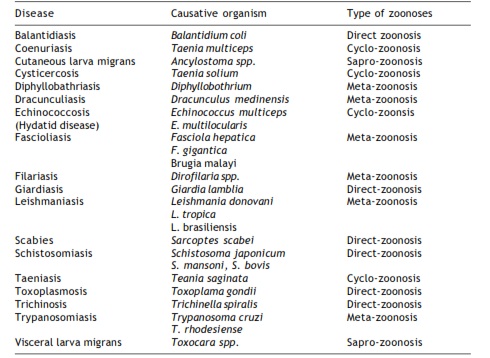
Some important zoonoses
Zoonoses are a heterogeneous group of diseases with a variety of causative agents. On the basis of causative agents, they are grouped into bacterial, parasitic, viral, rickettsial and other such groups.In general, parasitic zoonoses are usually food-borne, viz. meat-borne or fish-borne. These do not create epidemics and are often not fatal. However, they deplete nutrition and reduce working capacity of the victims. Bacterial zoonoses were at one time a world wide dread, for example plague, which was the cause of pandemics of Black Death of the past. With the production of effective vaccines, use of antibiotics and because of other measures taken, most of these are now subdued. Most of the existing bacterial zoonoses are related to occupation and the infection is mostly restricted to people at risk, e.g., anthrax and brucellosis.Viral zoonoses are the group of diseases that are mostly involved in high public risk and high case-fatality rate.It is not possible to describe each and every zoonotic disease. Only a few important zoonoses are described in Table
Rabies
Rabies or hydrophobia is a disease known from the dawn of the history. The infection is transmitted to animals or man by contact with the infected saliva, which may penetrate
the skin through scratch or a bite. Rabies is primarily a zoonotic disease and can infect a wide range of animals than other infectious diseases of man, amphibia and the higher vertebrates. It is the only communicable disease of man, which can be regarded as 100% fatal.Most of human cases of rabies are caused by the bite of an infected or rabid animal which is usually a dog or a cat. Man is an accidental host and is not a reservoir of the infection. Infection from man to man is very rare. Rabies in man occurs commonly in some areas of the world, particularly in Iran, India, the Philippines, North Africa and Thailand. Rabies is endemic in India and is important from the public health point of view.
Mostly dog remains the chief source of human exposure; cat is the second most common source, with other sources being cattle, jackals, raccoons and rodents. Wild animals trapped and sold as pets have on several occasions been responsible for human exposure to rabies. In Trinidad, the vampire bats transmit rabies. Rabies is also present among the fruit eating bats, which serve as reservoirs for the vampires.
Rabies in man or animal typically follows the bite of a mad dog or other animal. It is caused by a virus capable of invading the brain of animals. Once the virus enters the body through the bite on the skin, it travels by the way of the nerves to the brain and then to the salivary glands so that the saliva of the animal or the person can transmit the virus to other person or animal.
Due to involvement of the brain, man or animal with rabies behaves in an unnatural manner and remains in great distress. At this stage the rabid has a tendency to bite others without provocation. As the virus remains in high concentration in the saliva, infection may even spread by licking. Because of this the patient develops the fear of water which gives the condition its common name – hydrophobia. The patient passes into delirium with generalized convulsion. The outcome is invariably fatal.
The control of rabies is still a problem in India. This is in spite of knowledge of the disease. In our country only isolated attempts have been made to control rabies in Gujarat, Maharahstra, Kerala, and Madhya Pradesh, whereas many countries have either eradicated, or controlled it by strict law enforcement. The control of rabies should be done in association with creating awareness among people about the fatal character of the disease and a simple method of keeping away from the disease.
Following biting, once the symptoms of the disease begin, the disease invariably progresses to a fatal outcome. It is, therefore, imperative that treatment be given as soon as possible following the bite. Immediately after being bitten, the site should be treated with alcohol, iodine solution or carbolic acid after properly washing with soap and water. A physician should be informed and vaccination quickly arranged. Vaccination should be started immediately when it is known that the biting animal is rabid or when the bite is inflicted by wild animals. When the animal is available it should be carefully observed and vaccination should be started if considered necessary by the physician.In addition to these control measures, the provisions for diagnostic facilities and antirabies vaccines should be made available throughout the country. Satisfactory implemention of a control programme is based upon the help received from public health departments, Veterinary public health departments, vaccine manufacturers and above all cooperation from pet owners.
European bat lyssavirus infection: In Europe, European bat lyssaviruses (EBLVs) types 1 and 2 (genotypes 5 and 6, respectively) are closely related to classical rabies virus. EBLVs infect not only their primary hosts but also in rare circumstances, induce spillover infections to terrestrial mammals including domestic livestock, wildlife and man. Although spillover infections have occurred, there has been no evidence that the virus adapted to a new host. Human deaths from EBLVs have been reported.
Australian bat lyssavirus infection: Australian bat lyssavirus, identified in 1996, causes severe acute encephalitis. The virus is antigenically closely related to classical rabies virus in the genus Lyssavirus of the family Rhabdoviridae. However, classical rabies and Australian bat lyssaviruses are genetically distinct viruses. Human infections with Australian bat lyssavirus have been reported. The clinical signs are consistent with classical rabies infection and include diffuse, non-suppurative encephalitis. However, modes of transmission, pathogenesis, and geographic range still remain to be answered.