Mrs. M is a 35-year-old Hispanic female with no known past medical history; does not have a primary care provider (PCP). She presents to the emergency department with the following complaints: increasing fatigue, increasing thirst, unexpected weight loss of 30 lbs. She complains of numbness and tingling of the feet that keeps her awake at night. She states that she has a stabbing pain in her Rt calf when she walks and have noticed that her Rt foot swells when she has been on her feet. She denies any prescribed medication, except for regular use of Aleve for occasional headache, and denies any illegal drug use. She smokes 1 pks/daily. Social History: widowed, mother of three; is employed full time.
Upon admission to the ER the following vital signs are obtained: Wt: 255 lbs, reported Ht 5 ft 6 in; computed BMI 41.2; T. 102.2 º F; B/P 98/ 64; P.112 and irregular; R. 28; Pulse Ox on room air 90%.
Admission assessment reveals: Well-developed, morbidly obese female in acute distress, skin dry and hot, acetone odor to breath, PERRL, CN II-XII intact, Cardiac: S2 and S1 clearly audible, with S3 audible with patient lying on left side, no murmurs audible; irregular rate; peripheral pulses palpable 2+ with irregular rate noted. Lungs: Coarse wheezing heard throughout A&P, with expiratory grunting audible. Abdomen: rounded, no tenderness noted, bowel sounds audible x 4; Neurological exam: no deficits noted; G/U: deferred LMP: "2 weeks ago"; Extremities: 2 cm ulcer present on Rt lateral malleous with purulent drainage.
Initial orders: CBC with diff; Complete Metabolic Profile; 12-lead ECG, Stat BG; D-Dimer; CXR; Urinalysis; Arterial blood gas
Initial Laboratory findings: Only abnormal labs reported
CBC: WBC: 14.4 mm³; HCT 33.5 mL/dL: HGB: 10.2 gm/dL
CMP: SrCr: 1.6 mg/dl; BUN: 38 mg/dl ; K+: 5.8 mEq/L; Na+ 137mEq/L; CL: 104 mEq/L; Anion gap: 18 Mmol/min
Stat accucheck: BG 420 mg/dl
Arterial Blood gases: pH 7.21; pCO2 40; pO2 88, HCO3 16 mEq/L -
D-Dimer: positive; Urine: 4+ glucose, 3+ ketones,
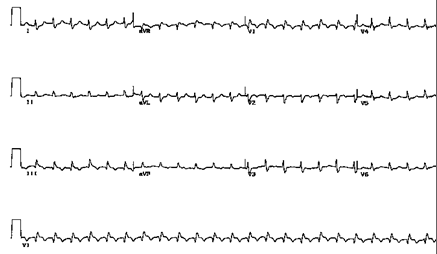
CXR: negative EKG: see below
Admit to ICU: 1400 cal Full liquid diet
Medication orders:
1). 2 L of Normal saline over 2 hours initially, then hydrate at 200 mL/hr N.S with 10 mEq KCL added.
2). Following fluid bolus: Regular insulin bolus IVP: 0.1 unit/kg, followed by a constant infusion at 0.1 units/kg/hr. Add 250 units Regular insulin to 250 mL N.S. Check BG q 1 hrs. Infuse at this rate until BG is less than 250 mg/dl.
3). Change IV solution to D5Wand infuse at 100 mL/hr as BG normalizes to 250 mg/dl. Then BG checks q 4 hrs and follow sliding scale:
Aspart Insulin SS with BG
180-200 2 units 301-350 8 units
201-250 4 units 351- 400 10 units
251-300 6 units > 400 give 12 units and call MD
4). Heparin bolus IVP 90 units/kg/dose.
5). Begin drip at 14 units/kg/hr. Add 25,000 units in 250 mL N.S. Run this rate for 4 hours, have lab draw aPTT, then follow the protocol for q 4 hrs aPTTs
Follow heparin protocol listed below
If aPTT < 35 sec Bolus: 80 units/kg, then increase rate by 4 units/kg/hr
If aPTT 33-45 sec Increase rate by 2 units/kg/hr
If aPTT 46-70 sec No change, repeat aPTT in 4 hours
If aPTT 71-90 sec Decrease infusion by 2 units/kg/hr
If aPTT > 90 sec Stop infusion for 1 hr, then decrease infusion by 3 units/kg/hr
Questions are to be answered thoroughly, be sure to include all components of the question.
1. Calculate the a) insulin bolus and b) drip rate of units/kg/hr and c) calculate the mL/hr for the insulin infusion
2. Calculate the a) heparin bolus, and b) heparin hourly rate and c) calculate the mL/hr for the heparin infusion:
3. Identify all abnormal laboratory findings: (hint: 12 abnormal labs): link abnormal labs to current condition/situation/provide rationale for abnormality.
4. After running the heparin drip for 4 hours at original order of 14 units/kg/hr, the aPTT remains 35 seconds.
a) What does the protocol state to do?
b) Calculate the bolus dose
c) How many mL/hr will the nurse set the infusion pump per the protocol direction?
5. Develop a discharge teaching plan based on the discharge medications. (Consider that this patient was on no medications prior to admission to hospital). Include in this discharge plan specifics regarding time of administration, indications for each new order and special instructions related to dietary restriction and subsequent lab monitoring.
Attach discharge teaching plan to the back of the case study
Discharge medications: Starlix 120 mg t.i.d. before meals
Lantus insulin 10 units at H.S.
Coumadin 5 mg M, W, F; 7.5 mg T,TR, 2.5 mg Sat, Sun
Lisonopril 20 mg daily
Norvasc 5 mg po daily
Acarbose 50 mg t.i.d.
Lipitor 10 mg daily
Read the following articles and answer the questions below:
Evidence based decisions for treatment with amlodipine (Norvasc) and atorvastatin (Lipitor)
Devabhaktuni, M. & Bangalore, S. (2009). Fixed combination of amlodipine and atorvastatin in cardiovascular risk management: Patient perspectives. Vascular Health and Risk Management, 5, 377-387.
6. How does amlodipine (Norvasc) impact the development of atherosclerosis?
7. What percentage of LDL-C reduction does atorvastatin (Lipitor) induce?
8. What were the most common treatment-related side effects of the combination of amlodipine (Norvasc) and atorvastatin (Lipitor)?
9. Which patients had the greatest reduction in HbA1c levels after 12 months on Glargine (Lantus)?
10. What percentage of patients achieved HbA1c levels of 7% in 12 months after switching from NPH to Glargine (Lantus)?
11. A reduction of 1% in HbA1c is associated with ______________ reduction in myocardial infarction, a ____________ reduction in all-cause mortality, a _______ reduction in microvascular complications, and a _______________ reduction in overall diabetic complications.
Clinical Pearls
1. Patients with type 2 diabetes may present with DKA. This condition seems to require some degree of insulin deficiency and is made more likely by concurrent illness
2. Prolonged hyperglycemia may lead to impaired endogenous secretion of insulin and reduced efficiency of insulin at the cellular level, a condition defined as glucose toxicity. This may result in insulin deficiency sufficient to cause DKA.
3. Hospital therapy for DKA in type 2 diabetes is the same for type 1 diabetes and hinges on fluid, electrolyte, and insulin repletion.
4. Outpatient therapy for decompensated type 2 diabetes following DKA will likely involve the combined use of short-and long-acting insulin.
5. As the effects of glucose toxicity resolve, a substantial proportion of patients with decompensated type diabetes will be able to discontinue insulin and resume the use of oral hypoglycemic agents to achieve glycemic control.