Reference no: EM132881263
BC6003 Advanced Infection and Tissue Science - London Metropolitan University
Case Study 1
A 26-year-old female post-graduate Zoology student went on an expedition to see the lowland gorillas in the Democratic Republic of Congo. She reported numerous insect bites while traveling but took anti-malarial prophylaxis. Approximately one week after returning home she developed a high fever of 410C and a pulse rate of 105 beats per minute.
About a month later, she started experiencing headaches, itchy skin, and swollen lymph nodes and sought medical attention. Posterior cervical lymphadenopathy was noted.
Laboratory data showed a haemoglobin value of 9 g/dL.
A blood specimen was prepared, smears made and stained with Wright-Giemsa before viewing under a microscope. Initial results were negative until the samples were prepared by microhaematocrit centrifugation, the results are shown in fig 1. Samples were also positive from the posterior cervical lymph node aspirate.
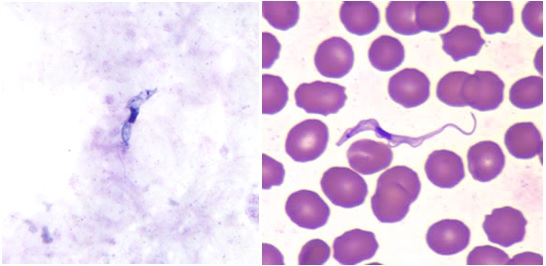
Figure 1: Thick (A) and thin (B) blood smears stained with Wright-Giemsa mag x1000.
Please answer the following questions:
1a) What is the diagnosis of the patient's condition?
b) What species of organism is likely to have caused this?
c) Give evidence from the case study to support your answers to a) and b).
2a) Why were thick and thin blood smears prepared?
b) Why did the samples undergo haematocrit centrifugation?
3. What further tests could be carried out?
4a) Outline the stages of this disease.
b) How does this differ from other varieties of the disease?
5. During the course of infection relapsing parasitaemia was observed.
Explain why this occurred.
6. What therapy should be recommended for the patient?
7. How could the disease be prevented?
Case Study 2
A 35 year old male from Manchester returned from a 6-month back packing trip, his travels included stops in Thailand, India, Pakistan, Egypt and Italy. He stayed at hostels or slept in the open and often bathed or drank unfiltered water from rivers and canals. During the trip general living conditions were often quite primitive.
During his trip, he suffered bouts of diarrhoea, fatigue, weight loss, occasional fever, and general malaise although visits to doctors during his triprevealed no specific diagnoses. Several months after he returned, he developed pain on urination, which was thought to be caused by prostatitis.
Two years after his trip, he developed frequency of urination, nocturia, and dark, grossly bloody urine. After cystoscopy, he was referred because of an apparent bladder tumour. Laboratory findings included a urinalysis which was normal apart from the presence of red blood cells and white blood cells. A cytological examination of the urine revealed no tumour cells. A bladder biopsy was performed, and numerous, small lesions were seen, which appeared to be below the mucosa. There were also some discoloured areas that were seen, but which did not appear specific to any particular condition. The following image was seen on biopsy:
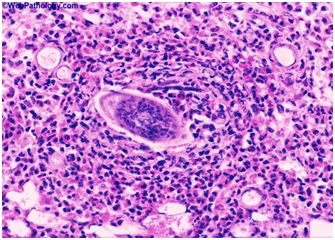
Figure 1. Giemsa stain of bladder tissue biopsy (150x magnification).
Please answer the following questions:
1a) What is the name of the disease the traveler acquired?
b) What species of organism is the most likely cause?
2. Why was the specimen sent to the cytologist?
3a) What is the nature of the lesions seen in the bladder?
b) What is their source?
4a)What is the distribution of the disease?
b) Approximately how many people suffer from this disease?
c) Where in his travels was the patient most likely to have acquired the disease?
5. Give an outline of the life cycle of this disease
6a) What would the patient have been given to treat this condition?
b) What side effects may have been experienced by the patient?
7. How is this disease controlled?